Can AI reduce ionizing radiation exposure in the diagnosis of CAD using CT?
By Filip Malawski
Coronary artery disease (CAD), commonly recognized as ischemic heart disease, is the leading global cause of mortality, responsible for 16% of all deaths [1, 2]. Among various diagnostic methods employed for CAD assessment, cardiac computed tomography (CT) has witnessed significant growth in recent times. This examination typically encompasses two main components:
- Coronary Artery Calcium Score: This CT scan is performed without the administration of a contrast agent, also referred to as a non-contrast scan. Calcified plaques are well visible. The coronary artery calcium score is routinely calculated based on these scans, reflecting the degree of calcification within the coronary arteries.
- Coronary Artery CT Angiography: This CT scan is performed following intravenous administration of a contrast agent to enhance the visibility of coronary arteries. This enables medical experts to assess blockages (stenosis) and blood flow through the coronary arteries.
Frequently, medical experts require information from both types of scans. Coronary arteries are best visualized when a contrast agent is used; however, calcified atherosclerotic plaques may be partially obscured by the presence of contrast agent. Therefore, a separate non-contrast CT scan is routinely performed. CT scanning, a 3D form of X-ray imaging, uses ionizing radiation, which inherently poses risks to patients. Therefore, radiation exposure should be minimized to the lowest levels adequate for diagnosis. In simpler terms, fewer CT scans for a patient equate to a safer approach.
AI’s potential to analyze coronary arteries and plaque with a single CT scan
A pertinent question emerges: Is it truly necessary to perform two distinct CT scans to examine both coronary arteries and calcified plaques? Thus far, this has been the medical standard, as human experts cannot extract all necessary information from a single type of scan (either contrast or non-contrast). However, what role can artificial intelligence (AI) play in this medical application? We are already aware that, in some instances, deep learning algorithms can analyze medical images beyond the capabilities of the human eye [3]. Can AI be efficiently employed here as well? At Graylight Imaging, we embarked on an investigation to test the hypothesis that AI-enabled automatic analysis of a single contrast CT scan can provide information not only about coronary arteries but also calcified plaques as well.
Can AI Algorithms confirm the effectiveness of contrast CT scans for precision heart disease risk assessment?
A frequently used metric for assessing coronary artery calcification is the coronary artery calcium (CAC) score computed using the Agatston method [4]. This score is derived from the volume and density of plaques detected in a non-contrast CT scan and signifies the amount of calcified plaques in coronary arteries, corresponding to the risk levels of coronary artery disease. These risk levels, in turn, could determine patient treatment. Consequently, our goal was to develop an AI algorithm capable of determining risk levels based solely on a contrast CT scan, obviating the need for an additional non-contrast scan. Employing state-of-the-art deep learning techniques and problem-specific machine learning approaches, we assessed risk levels in contrast CT scans and compared them with our ground truth – risk levels determined by medical experts in corresponding non-contrast scans. Our results were evaluated using Cohen’s kappa coefficient (κ), a widely-used statistic for measuring the reliability of two rating methods. We obtained κ = 0.8, indicating a very substantial level of agreement [5]. The results of our study suggest that a single contrast CT scan may often be sufficient for patients with suspected or known coronary artery disease.
AI algorithms compare calcium plaque detection in contrast vs. non-contrast CT scans
Below, we present an illustrative example of calcified plaques detected in non-contrast (left images) and contrast-enhanced CT scans (right images) of the same patient. It is important to note that non-contrast scans are typically conducted at lower resolution, resulting in plaques appearing more bulky compared to those in contrast scans. Coronary arteries, depicted in gray, are well visible in the contrast scan but only partially in the non-contrast scan.
These advancements driven by AI help make diagnosing heart problems more accurate and choosing the right treatments better. As technology gets better, we can expect even more detailed information to guide medical decisions.
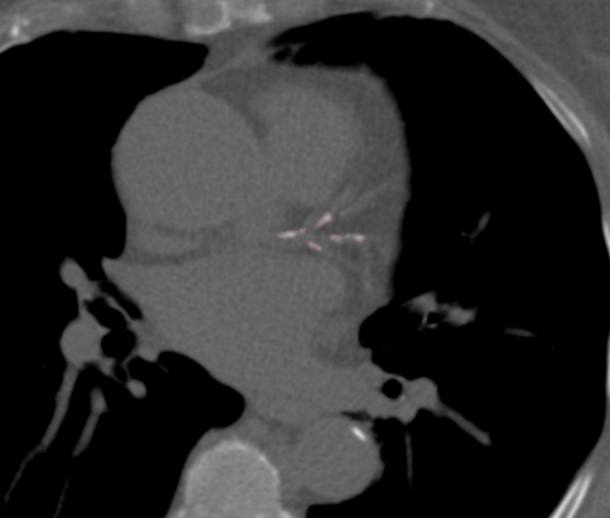
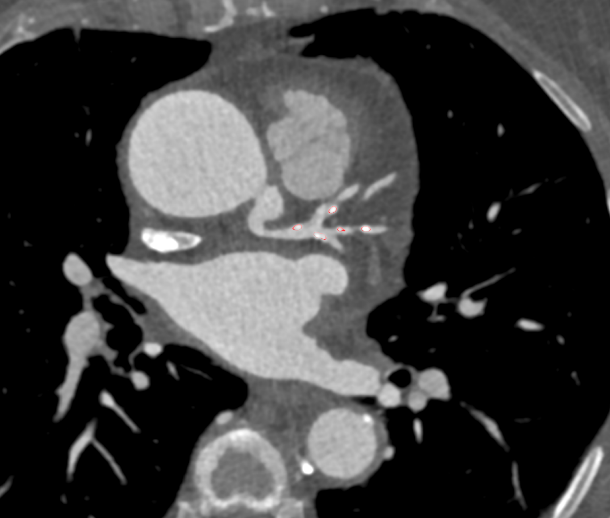
Non-contrast calcium score CT scan with highlighted calcifications ≥130 HU within the left coronary artery (left image). Contrast-enhanced CT scan at the corresponding level depicting calcified plaques detected by the AI algorithm in the same location (right image).
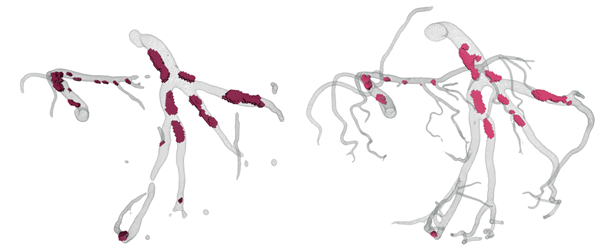
3D reconstructions of coronary arteries and detected calcified plaques in non-contrast (left image) and contrast-enhanced (right image) CT scans of the same patient.
AI innovations cut radiation exposure in coronary artery disease diagnosis
AI algorithms can assist in interpreting medical images, enabling more precise diagnoses and minimizing the necessity for repetitive scans. Through accurate image analysis, AI can offer insights into the severity and scope of coronary artery disease, aiding healthcare professionals in making informed decisions with limited radiation exposure.
In conclusion, our research demonstrates that AI’s potential lies in its capability to improve image quality, optimize radiation dosage, and enhance diagnostic accuracy. These advancements collectively contribute to the reduction of ionizing radiation exposure during the diagnosis of coronary artery disease.
References:
[1] https://ourworldindata.org/causes-of-death
[2] https://www.cdc.gov/heartdisease/coronary_ad.htm
[3] https://www.diagnosticimaging.com/view/autonomous-ai-nearly-27-percent-higher-sensitivity-than-radiology-reports-for-abnormal-chest-x-rays
[4] https://radiopaedia.org/articles/agatston-score
[5] https://ncbi.nlm.nih.gov/pmc/articles/PMC3900052/