AI in medical image analysis can boost ROI in clinical research
Return on investment: patient response assessment with AI
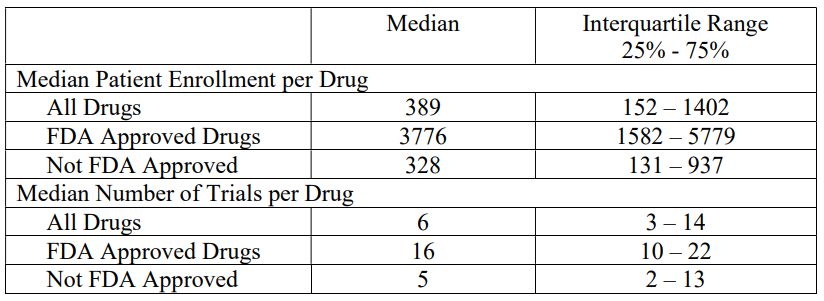
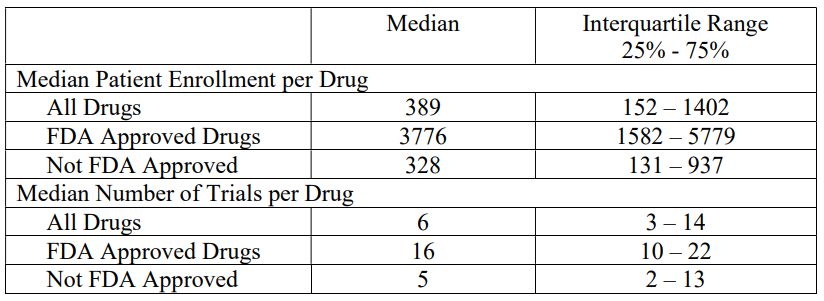
Return on investment, ROI in clinical research is clear-cut when expenses and income are readily assigned. So, let’s do the math. And – in order to do this – let’s assume some values. Let’s use an average cost of $200 for an imaging examination with a radiologist’s report [1]. Based on data from the U.S. Department of Health and Human Services [2], let’s assume an average of 389 patients participating in a trial. Let’s consider that each patient will need to undergo 5 scans during the research.
200$ * 389 * 5 = 389 000$
This is a relatively straightforward calculation. You may even evaluate its validity with data from past trials. What if only a part of this money was enough to create an algorithm that would measure a patient’s response to a substance in a repeatable, objective, and quantitative way? It could be used repeatedly and guarantee the same performance, providing analysis of a single study in just a few minutes. This is not a pious wish, but a real possibility that we are bringing to the table with the offer of custom algorithms development.
Maintain the status quo. What is the cost of doing nothing?
Hesitation or uncertainty related to the incorporation of artificial intelligence algorithms remains present in the scientific, clinical, and pharmaceutical environment. And it is very good that we trust medical knowledge and years of experience more than almost incomprehensible software. The only question is whether we can afford to maintain this status quo in the long run.
The radiologist shortage is a well-known, complex issue with multifaceted impacts. It requires a proactive approach, because the cost of doing nothing may strike in the future with redoubled force. In Europe, the average stands at a mere 12.8 radiologist for every 100,000 citizens [3]. The US grapples with projections of a clinicians’ deficit ranging from 10,300 to 35,600 by 2034 [4].
The CDC reports a 5% annual increase in imaging studies, while radiology residencies only grow by 2% [5]. This mismatch further strains the existing workforce, leading to longer wait times, delayed diagnoses, and potential unwanted compromises. It also influences the time needed for clinical research and entails additional costs. We can already talk about the snowball effect and the problem will only grow.
Think about the actual savings on the fixed costs associated with medical imaging analysis timeline and potential ROI in clinical research. If a couple of months can be cut from the clinical research, that’s a couple fewer months of financing the study’s fixed expenses.

Can AI algorithm fix this problem just like that? Surely not entirely, but it might be an impactful milestone.
Testing AI’s limits and reliability in pharma research
The U.S. Department of Health and Human Services report mentioned above cited a median of 389 for all studies analyzed. Interestingly, for studies that received FDA approval, the median is 3,776 patients, and the upper quartile in this group is close to 6,000. Substituting these data into the formula yields astronomical numbers.
Not to mention the obvious challenges: enrollment and retention bottlenecks, patients becoming unresponsive during the clinical trial or site under-enrollment etc. But it’s not just about simple multiplication. Analyzing patient responses requires consistency and repeatability. Imagine two radiologists analyzing the same scan. Or even the same radiologist analyzing several studies of the same patient. Subjectivity’s shadow is something that is permanently inscribed in nuances of radiology, but which at the same time can determine the effect of the research, even the most expensive one.
Interobserver variability and intraobserver variability were the subjects of our previous post, so we won’t focus on them now. But if your doubts linger about AI’s ability to produce reliable, consistent results for the same patient with the sustained accuracy needed for longitudinal tracking, we did a test. We investigated these questions and tested one of the algorithms we built on real-world data. It is all described in mentioned post.
Time is money. Get the ROI in clinical research
Imagine fast and reliable medical image analysis. Thousands of patient scans analyzed with unprecedented repeatability and objectivity. Imagine identifying subtle trends and patterns human eyes might miss. Imagine boosting your clinical trial efficiency and saving money at the same time. This isn’t science fiction.
Our earlier point holds: thanks to medical algorithms you may save real money. Ready to see the difference AI can make in your research? Let’s discuss your specific needs and talk about how AI algorithms can transform your work.
FAQ
What is the return on investment (ROI)?
The return on investment (ROI), also known as rate of return (ROR) is a vital metric that helps you assess the profitability and overall success of the investment by measuring the percentage gain or loss over a specific period. While calculating ROI can sometimes be complex, it unlocks valuable insights into the performance of your investments.
What is the internal rate of return (IRR)?
Internal rate of return (IRR) helps you assess the potential profitability of investments or projects. It acts like a yardstick, allowing you to compare different projects within the same company or even across different investments. Generally, a higher IRR indicates a more attractive opportunity, promising a potentially higher return on your investment.
What is the absolute return on investment?
Absolute return tracks the raw percentage gain or loss of your investment over time, ignoring any costs involved. On the other hand, ROI factors in those costs, offering a clearer picture of your actual profit relative to what you invested.
What is the relative return on investment?
Relative return tells you how your investment performed compared to a similar benchmark. Unlike absolute return, which shows just the raw gain or loss, relative return reveals how your investment fared against the competition, making it crucial for understanding its true performance.
References
[1] The data presented is based on our experience in executing projects for the pharmaceutical industry.
[2] Examination of Clinical Trial Costs and Barriers for Drug Development, U.S. Department of Health and Human Services, https://aspe.hhs.gov/reports/examination-clinical-trial-costs-barriers-drug-development-0
[3] https://www.marwoodgroup.com/wp-content/uploads/2022/09/European-Radiology-Services_June-2022.pdf
[5] https://www.itnonline.com/article/minding-gap-strategies-address-growing-radiology-shortage